Earlier this year, my collaborators and I announced that mRNA vaccines—made famous by COVID-19 and recently awarded the 2023 Nobel Prize in Medicine—showed promise as a therapy for pancreatic cancer in a phase I clinical trial. The collaboration underlying this work originated, in part, from a meeting at IAS on Valentine’s Day of 2015, a day that featured a cold extreme enough to freeze the Institute pond. The grim weather also, advantageously, confined indoors a group of mathematicians and theoretical physicists (for whom being cooped up was not unusual), as well as oncologists (whose inability to travel forced them to settle into Institute culture in a way their schedules do not typically allow). This collection of individuals was convened for a series of meetings organized by Arnold Levine, Professor Emeritus in the School of Natural Sciences, to hear from speakers on emerging topics in cancer research that seemed poised for productive collaboration between quantitative scientists and oncology researchers.
I was a Long-term Member in the School of Natural Sciences from 2008 to 2013. The main theoretical question I focused on while at the Institute (and still grapple with today) concerns the immune system. Why does it target one particular molecular feature over another, what does that tell us about genome evolution, and how does that selection affect the evolution of cancer and viruses? In short, I am interested in the theory of self versus non-self discrimination.
Broadly speaking, the immune system works by identifying the presence of pathogens—i.e., that which is not “self”—in the body, in order to combat infection. It seeks to complete this process while leaving cells belonging to the body—i.e., those which can be described as “self”—to complete their normal functions. But, because the immune system’s machinery for discriminating between these two states is imperfect, and because, as we and others have shown, pathogens often do their best to mimic that which is self in order to survive, this process is not always successful. Greater understanding of how the immune system discriminates between these two is important in helping the immune system more successfully complete its task.
My theoretical work at the Institute and my continued collaborations there, as in the aforementioned series of meetings, led, perhaps unexpectedly, to an opportunity to apply this line of questioning to cancer. The Institute for Advanced Study allowed for time to reflect on the theoretical, abstract principles that underlie new empirical findings in a way that is difficult to achieve elsewhere. It is also a powerful location for convening small and mesoscale meetings on topics that bring together people to talk to, rather than past, one another. The consequences are not always obvious at the time, but, occasionally, something particularly useful can emerge.

The immune system’s successful targeting of “non-self,” namely the non-specific features that differ between ourselves and pathogens over evolutionary time scales (innate immunity) and the specific features learned within our lifetime (adaptive immunity), is necessary to combat infection by pathogens, like COVID-19 or influenza. My research at IAS initially focused on innate immunity. The innate immune system is a genetic system that recognizes patterns that discriminate pathogens from the organisms they infect. At the forefront of innate immunity are pattern recognition receptors that recognize features many pathogens share. For instance, when influenza (a virus with a genome made from RNA, instead of DNA like ours) replicates, it—like any other virus—needs to copy itself and, in doing so, temporarily makes long double-strands of RNA at a length that is rare in our genome. Many organisms have evolutionarily conserved receptors that sense double-stranded RNA in their cells, a hardwired example of self versus non-self discrimination by the innate immune system. By focusing on such non-specific molecular features shared by broad classes of pathogens, the innate immune system is often the first line of defense against a new infection.
During my time at IAS, I studied how the innate immune system alters virus evolution when a virus changes its host, such as during the 1918 influenza or COVID-19 pandemic. One organism’s genetic definition of non-self can differ from another organism’s definition. For instance, the set of innate receptors in birds (the hosts of influenza) have some differences from those in humans. I, along with other Members, showed how these receptor differences can enforce mimicry: when a virus enters a new host, its genome, to evade detection by its new hosts’ receptors, evolves to look more like the genome of its new host.
When I arrived at the Institute, I worked with Members Raúl Rabadán (2003–09) and Gyan Bhanot (1981–84, 1987–94, 2002, 2003–10) to study the evolution of influenza in humans since 1918. We used this evolutionary history to elucidate how mimicry evolves due to innate immune system differences between humans and birds. Such differences, therefore, also tell us quantitative differences between how self is defined in those two hosts. Using this information in conjunction with inferences of the patterns viruses avoid as they evolve, one can predict which patterns the innate immune system targets. I worked with IAS Members Rémi Monasson (2009–11) and Simona Cocco (2009–11) to build a mathematical theory and predictive evolutionary models around this topic during the end of my time at IAS.1
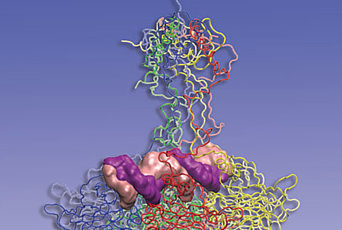
Pathogens can adapt rapidly, their genomes mutating at a faster rate than ours, and an immune system based only on innate immunity would be vulnerable. The adaptive immune system is the arm of our immune system that detects features in pathogens that are not well conserved across evolution. The T cells (and B cells) of the adaptive immune system recognize antigens, namely short protein regions in pathogens, with great specificity over the course of our lifetime and, in some cases, commit those antigens to memory. Likewise, a vaccine can educate the adaptive immune system as to what antigens it may encounter in the future.
Here’s loosely how it works: proteins inside cells are cut into short fragments, called peptides, and are presented on the cell’s surface, be they proteins required for normal cell functioning or non-self proteins, like antigens. T cells, via an evolutionary innovation, can seek these antigens and, upon recognition, can destroy the cells containing them. However, the antigen presentation machinery does not discriminate well between presenting self peptides and pathogen peptides. A successful immune response would disproportionately recognize these non-self peptides and eliminate the cells which contain them, while avoiding eliminating cells that only presented self peptides. If the immune system erred on the side of the latter, it would attack our own tissue in a wave of autoimmunity, while if it erred on the side of the former, viruses could gain an advantage by mimicking self-proteins.
How this trade-off is balanced—to recognize infection while avoiding self-destruction —is the subject of the theory of immune tolerance, the mechanisms by which the adaptive immune system learns to inhibit the immune response against self peptides. In the thymus, T cells that recognize self peptides can be eliminated. It had been previously thought that this training of T cells in the thymus was nearly exhaustive, meaning the immune system would play little role against that which is very closely related to self, and would favor peptides dissimilar from self (leaving an opening for rapidly evolving viruses to mimic self peptides).
But our empirical understanding of tolerance has changed fundamentally since theorists first attempted to create mathematical measures quantifying non-self several decades ago. Over the last few decades, a different picture has emerged, one in which many T cells that are capable of recognizing self or near-self peptides survive elimination in the thymus and are, instead, held back by mechanisms of a process called negative regulation. Negative regulation, rather than just eliminating T cells that recognize self (or near-self) peptides, instead holds them in check. This means that, if negative regulation could be suppressed, the T cells that recognize near-self peptides could be deployed against pathogens—and cancer.

By starting out as self and evolving in ways the immune system may recognize as “non-self,” cancer evolution can illuminate the very boundary between the two states. As cancer cells evolve, they accumulate mutations in their DNA. Those mutations create changes in proteins that give cancer cells their pathological selective advantage over neighboring cells. Yet, at the same time, the very same mutations can make the proteins of those cells different than the proteins the immune system was trained on. These new antigens, created during tumor evolution, are called neoantigens.
Many neoantigens differ from self by only one mutation. Given this close similarity to self-proteins, the older understanding of tolerance could imply this may be too self similar to mount an effective immune response. Indeed, for many years it was thought that the immune system did not play much of a role in cancer evolution. A fundamental change was the discovery of immune checkpoints, a breakthrough which received the 2018 Nobel Prize in Medicine. This revealed that part of the reason why the immune system could not recognize cancer cells was not that T cells capable of recognition were completely absent, but rather that they had been inhibited via negative regulation. Once negative regulation was restrained, immune recognition of some cancers was now possible.
In the old model of hard tolerance, it may have seemed equally unlikely that the immune system would detect any peptides that are similar to self. However, we have posited that the significance lies in the specific qualities of neoantigens the immune system is able to recognize as cancer cells evolve. In other words, our notion of antigenic distance from self is non-trivial. For the next phase of my research, after IAS, I chose to study how the adaptive immune system recognizes peptides in cancer, investigating what biophysical and chemical features make something that was once self—the proteins in a cancer cell—appear as non-self to the immune system.
That fundamental understanding can then be acted upon by trying to enhance the immune system’s capability of recognizing tumors. One logical application is in the selection of targets in an anticancer vaccine, which brings us back to the frigid meeting at IAS. At that meeting, Jedd Wolchok (then at Memorial Sloan Kettering), who had led some of the first clinical trials in immunotherapy, described recent findings on neoantigens and response to immunotherapy. I spoke with him about building mathematical models around immunotherapy response based on the immune system’s ability to differentially recognize neoantigens, work on which I then collaborated with past Research Associate (2014–18) Marta Łuksza (to whom I had been introduced by Stanislas Leibler, Professor in the School of Natural Sciences). Shortly thereafter, Jedd’s colleagues at MSK, led by Vinod Balachandran, reached out to me to share evidence that, in pancreatic cancer, long-term survivors had unusual immunological activity.

Pancreatic cancer had often been thought of as an immune desert, with little penetrance of the immune cells needed to combat a tumor. It is generally nonresponsive to immunotherapies—it has relatively few alterations in its DNA and, therefore, less of a chance of generating neoantigens that could elicit an immune response. Many vaccination efforts had, accordingly, been focused on cancer types where the role of the immune system had been better established, such as melanoma and lung cancer. However, the tumors of long-term survivors of pancreatic cancer were showing evidence of T cell infiltration. When our models were applied to this data, we were able to show that the evolution in pancreas tumors of long-term survivors was consistent with selection on neoantigens. Our team has continued to develop and extend such “neoantigen quality” models to understand which features make an altered peptide recognizable to the immune system in a way that alters cancer cell fitness.
We hypothesized that our results could be an example of spontaneous recognition of neoantigens in a rare subset of patients, a kind of “auto-vaccination.” If, in rare cases, the immune system may shape the evolution of pancreatic tumors, perhaps we could boost the immune response to a larger set of antigens in more patients through vaccination. Vinod and I immediately applied for funding to support a clinical trial (which Vinod led) and analyze the results. Many platforms were considered, but it was decided that mRNA vaccines made a promising candidate after a set of meetings with the groups at BioNTech and Genentech.
Each of the 16 trial patients had their tumor removed and flown to Mainz, Germany where a personalized mRNA vaccine was created based on up to 20 mutations specific to that tumor. The trial showed immunological responses in half (of the 16) patients treated. Additionally, our study of the trial’s results contained a first of its kind mathematical analysis of the dynamics of T cells responding to a cancer vaccine. While these initial results should be interpreted with caution, as this was a phase I clinical trial,2 they offer precious data into the action of mRNA vaccines in the setting of pancreatic cancer.
The above work is a recent example of two of the many features that make the Institute special. The trial was conceptualized in 2016, well before COVID-19, when mRNA technology was not particularly well known to the public and its basic effectiveness as a vaccine platform was far less clear. Moreover, as stated above, the decision to attempt vaccination in pancreatic cancer was, in many ways, counterintuitive. So, what was the research path that led to such an unusual effort? It was, in part, due to the unique IAS atmosphere: a line of theoretical inquiry initiated at the Institute, and a set of meetings held there to create collaboration in emerging areas of research.
Benjamin D. Greenbaum was the Eric and Wendy Schmidt Long-term Member in the Simons Center for Systems Biology from 2008–2013. He is an Associate Member of Memorial Sloan Kettering Cancer Center (MSKCC) and an Associate Professor of Physiology, Systems Biology and Biophysics at Weill Cornell Medicine. He has a Ph.D. in theoretical physics from Columbia University. He currently works on how the innate and adaptive immune system impact cancer and virus evolution, how immune interactions effect models of cancer cells fitness, and the role of repetitive elements in cancer and genome evolution. At MSKCC, he started a programmatic effort in Computational Immuno-oncology and is helping to translate his work and that of colleagues into next generation immunotherapies, particularly cancer vaccines. He continues to work on a number of theoretical topics related to the immune system and genome evolution.
1. In a story for another time, this work has also had surprising and profound applications in understanding how cancer interacts with the innate immune system.
2. Meaning it had no control arm and, thus, shows correlation and not causation.